As told by Lauren, a nurse practitioner residing in Rochester, NY, and a Doctor of Nursing Practice student at Duke University School of Nursing.
It was after nine in the evening when my phone rang. It was my best friend, calling a little later than usual. I had “Married at First Sight” on TV—my guilty pleasure—and was relaxing on the couch. Her cheerful voice came through as always, but this time her first words were different: “So, I’m calling you for medical advice…” Those words would come to haunt me.
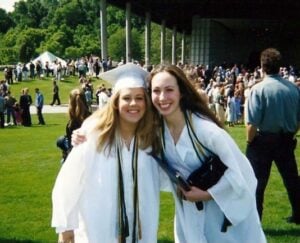
My best friend Susan and I had known each other since Girl Scouts. We graduated from high school together in upstate New York and stayed close even after she moved to Charlotte, North Carolina. Just 12 hours after that phone call, Susan was gone. She died from a massive blood clot that had formed in her leg and traveled to her lungs, blocking blood flow and stopping her heart. She was only 35—radiant, funny, smart, and generous.
That night, she told me she’d been having chest discomfort for a week. It had gone away, then returned. As we talked, I tried to think through possible causes based on my experience working in the nursing field.
Could it be anxiety? Maybe her asthma is acting up? I asked if she’d used her inhaler, and she had. Could it be costochondritis—which is inflammation in the chest muscles or cartilage? I told her to try a little more ibuprofen.
A blood clot? Probably not, I thought. She didn’t smoke, wasn’t over 35, and saw her doctor regularly. No family history of clots. She wasn’t struggling to breathe and sounded fine. “Perhaps see how you feel in the morning,” I suggested.
But the next morning, the pain was worse. It hurt when she breathed in and out. She fainted getting out of bed. Susan died at the hospital around 9 a.m.
According to the National Blood Clot Alliance, about 273 people in the U.S. die every day from blood clots. Birth control that contains estrogen—like the pill, patch, or vaginal ring—can increase that risk. Susan was taking a combined birth control pill (one that has both estrogen and another hormone called progestin). Her healthcare provider had never mentioned that these pills could increase the chance of dangerous blood clots, known medically as DVTs (deep vein thrombosis, or clots in the leg) and PEs (pulmonary embolism, or clots in the lungs).
Susan had recently gained some weight and also taken a long car ride to the mountains, factors that can also raise the risk of clots. By the time anyone realized what was happening, it was too late. I falsely thought genetic clotting disorders—conditions that make some people form clots more easily—usually show up earlier in life. I assumed these genetic conditions would be known by the time someone was in their early 20s. I was wrong.
After Susan’s death, I started following the National Blood Clot Alliance and was shocked to see how many young women had similar stories. In many cases, the only thing they had in common was taking birth control with estrogen. These pills can act as a trigger for a clot in someone who has an undiagnosed genetic condition that makes their blood clot more easily—and many people don’t even know they have one.
While estrogen-containing birth control helps many women, I believe Susan might still be alive today if she hadn’t been taking the pill. I’ll never know for sure whether she had a hidden genetic clotting condition. According to the National Institutes of Health, about 5% of people of European descent have factor V Leiden, the most common inherited clotting disorder. There are many other inherited or acquired conditions that can increase clotting risk.
My message is this: Know your risks. Blood clots can happen to anyone, at any stage of life. Learn the warning signs of blood clots, discuss alternatives to estrogen-based birth control with your healthcare provider, and whether a blood screening test before starting any medication that might raise your blood clotting risk may be appropriate. Activated protein C resistance assay is a single blood test that can screen for favor V Leiden.
During long car rides or flights, wear compression socks, stretch your legs, and take breaks to walk around. Pregnancy and surgery can also increase risk—but even if you don’t have any risk factors, don’t ignore symptoms. Chest pain, shortness of breath, or swelling in your legs can be life-threatening — get medical help immediately. It could be lifesaving




