Expecting or recently had a baby?
Don’t let a blood clot spoil your joy.
Don’t let a blood clot spoil your joy.
If you are expecting or recently had a baby, you know that it can be an exciting and joyful time. From doctor’s visits, where you might catch the first glimpse of your developing baby during an ultrasound, to decorating the nursery and picking out precious little baby clothes. Enjoy all of these special moments and plans.
As you prepare for the day when your baby arrives, it is important that you take care of yourself. There is one key health issue that many women who are expecting a baby might overlook: dangerous blood clots.
Pregnancy, childbirth, and the three-month period after delivery are times when there are major risks for the development of dangerous blood clots. With the right information and a prevention plan, blood clots may be prevented.
Get the facts

A woman’s blood naturally clots more easily during pregnancy to help her body prepare for blood loss during childbirth. Other factors unique to pregnancy can contribute to the development of blood clots:
Blood flow slows later in pregnancy, due to pressure on a woman’s blood vessels from the growing baby.
A woman may experience injury to veins during delivery or surgery.
Prolonged immobility due to bed rest during pregnancy or while recovering from childbirth can cause blood to pool and slow blood flow.


Dangerous blood clots can affect you and your developing baby.
Blood clots can form in the deep veins of a woman’s legs or arms and block the flow of blood through the vein. Left untreated, blood clots in the legs or arms can break off and travel to the lungs, which can be life threatening.
Blood clots during pregnancy also can be dangerous for the developing baby because they can cut off blood flow to the developing baby.
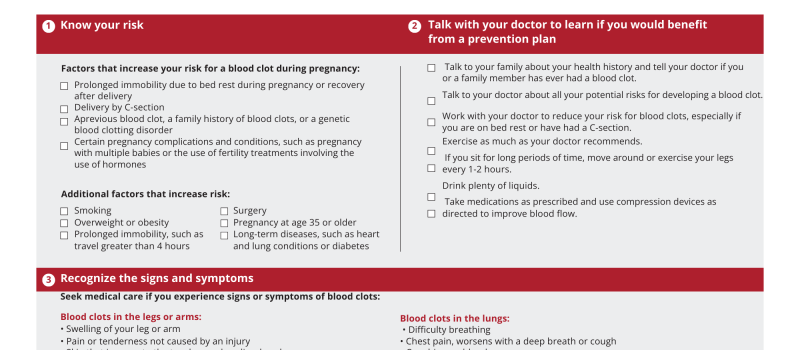
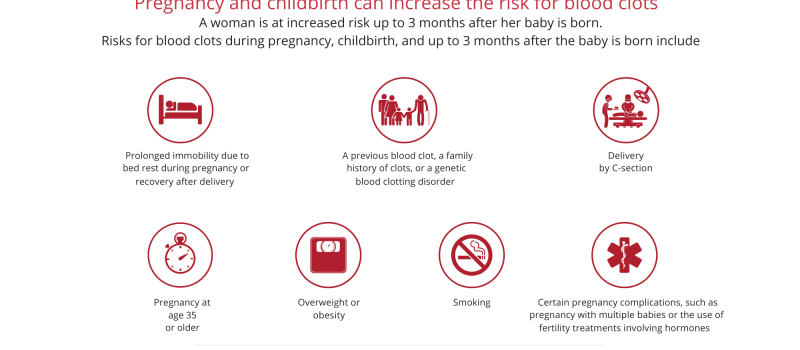
Risks for blood clots during pregnancy, childbirth, and up to three months after delivery.
Blood Loss
Blood naturally clots more easily during pregnancy to prepare for blood loss during childbirth
Immobility
Prolonged immobility due to bed rest during pregnancy or recovery after delivery
Family History
A previous blood clot, a family history of blood clots, or a genetic blood clotting disorder
Surgical Delivery
The surgical delivery of a baby by C-section
Other Complications
Certain pregnancy complications and conditions, such as pregnancy with multiple babies or the use of fertility treatments involving hormones
Other factors that can increase a woman’s risk for blood clots
during pregnancy and the postpartum period
during pregnancy and the postpartum period
• Smoking • Overweight or obesity • Other prolonged immobility, such as travel for more than four hours • Surgery
• Pregnancy at age 35 or older • Long-term diseases, such as heart and lung conditions, or diabetes
As you prepare for baby,
don’t forget to take care of yourself.
don’t forget to take care of yourself.
A woman is at increased risk for a dangerous blood clot throughout her pregnancy, during childbirth, and up to three months after her baby is born.
When you take care of yourself, you take care of your developing baby too.
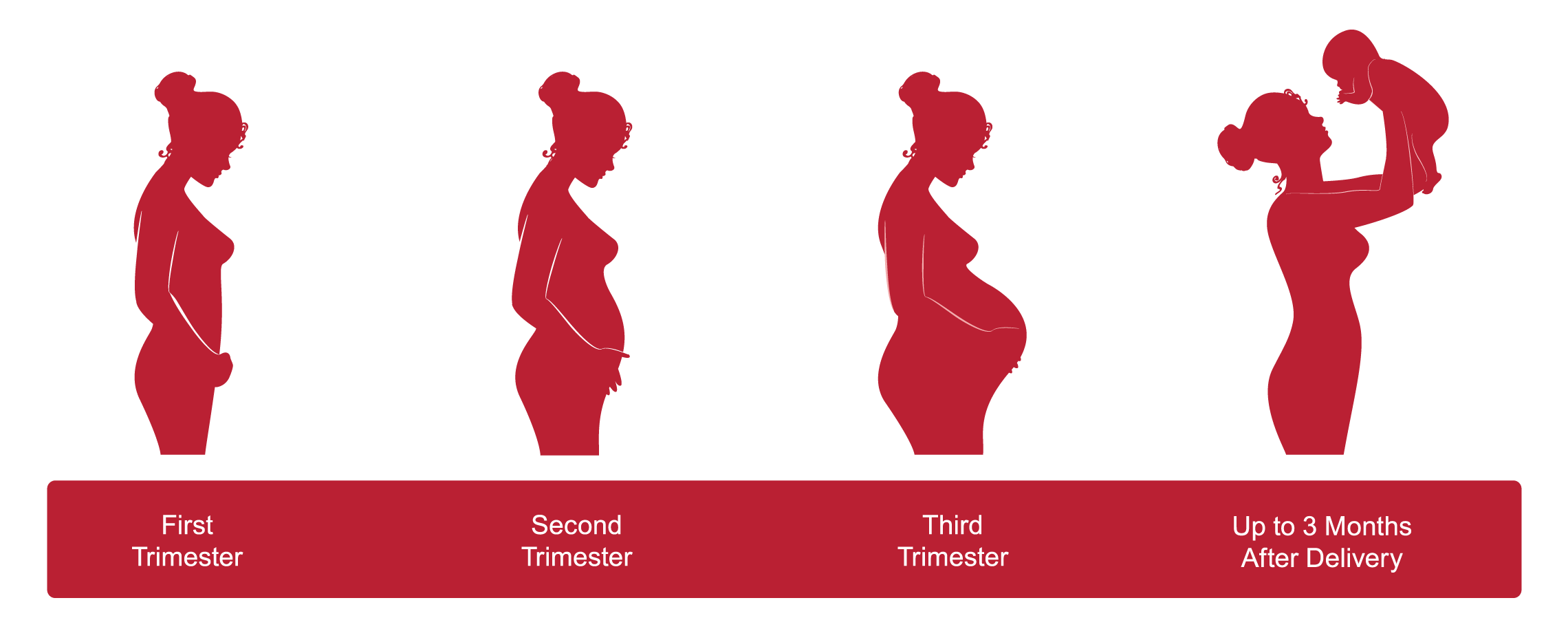
When blood clots connected to pregnancy form in the legs or lungs, one-half of them occur during pregnancy, and one-half occur in the three-month period after the baby is born.
Cherish the experience of pregnancy and childbirth.
Don’t let a blood clot spoil your joy.
Talk to your doctor to learn if you might benefit from a blood clot prevention plan.
Don’t let a blood clot spoil your joy.
Talk to your doctor to learn if you might benefit from a blood clot prevention plan.
Talk to your family about your health history and tell your doctor if you or a family member has ever had a blood clot.
Talk to your doctor about all of your potential risks for developing blood clots.
Work with your doctor to reduce your risk for blood clots, especially if you are on bed rest, have a history of blood clots, or have had a C-section.
Exercise as much as your doctor recommends. If you sit for long periods of time, move around or exercise your legs frequently.
Drink plenty of liquids. Recommend that women drink 10, eight-ounce glasses of liquid every day while pregnant, and 12-13 glasses of liquid every day while breastfeeding.
Take medications and use compression devices as prescribed.
Women at increased risk for dangerous blood clots, or previously diagnosed with a blood clot, should discuss options to prevent blood clots with their doctor.
If a pregnant woman is at higher risk for developing blood clots, her doctor may prescribe one or more methods to prevent blood clots during her pregnancy and up to three months after her baby is born.
There are two safe and effective methods of blood clot prevention for pregnant women at increased risk for blood clots :
- Compression stockings or compression devices that help to keep blood moving in the legs.
- An anticoagulation medicine, also called a blood thinner, that does not affect the developing baby.

Tell your doctor if you experience any of the signs or symptoms of a blood clot.

SYMPTOMS OF A BLOOD CLOT
IN THE ARM OR LEG MAY INCLUDE
IN THE ARM OR LEG MAY INCLUDE
– Swelling –
– Pain or tenderness not caused by injury –
– Skin that is warm to the touch –
– Redness or discoloration of the skin –
– Pain or tenderness not caused by injury –
– Skin that is warm to the touch –
– Redness or discoloration of the skin –
If you have these signs or symptoms, alert your doctor as soon as possible.
SYMPTOMS OF A BLOOD CLOT
IN THE LUNG MAY INCLUDE
IN THE LUNG MAY INCLUDE
– Difficulty breathing –
– Chest pain that worsens with a deep breath or cough –
– Coughing up blood –
– Faster than normal or irregular heartbeat –
– Chest pain that worsens with a deep breath or cough –
– Coughing up blood –
– Faster than normal or irregular heartbeat –
Seek immediate attention if you experience these signs or symptoms.
Stop the Clot, Spread the Word®
The National Blood Clot Alliance and the Centers for Disease Control and Prevention are working on this important public health campaign to get the word out about blood clot risks and the signs and symptoms of blood clots.
You can be an important part of this education campaign by helping us
SPREAD THE WORD®
Please share this page
Other campaign items to share
For more information about blood clots, visit:
The information and materials on this site are provided for general information purposes only. You should not rely on the information provided as a substitute for actual professional medical advice, care, or treatment. This site is not designed to and does not provide medical advice, professional diagnosis, opinion, treatment, or services to you or any individual. If you believe you have a medical emergency, call 911 immediately.
Stop the Clot, Spread the Word® is a public education campaign made possible by funding provided to the National Blood Clot Alliance by the Centers for Disease Control and Prevention under Cooperative Agreement number 1U27DD001153-02.


The mark ‘CDC’ is owned by the US Dept. of Health and Human Services and is used with permission. Use of this logo is not an endorsement by HHS or CDC of any particular product, service, or enterprise.